Webinar Series Targets Workforce Burnout
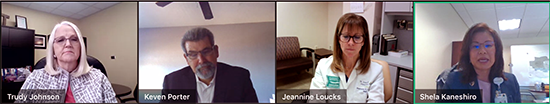
Participants at the HASC session included (from left) Dignity’s Trudy Johnson, HASC’s Keven Porter (moderator), Providence St. Joseph’s Jeannine Loucks, and MemorialCare’s Shela Kaneshiro.
The ongoing pandemic is driving workers from frontline care, stretching teams thin and placing more load on current staffers, a panel of nurse leaders told A Workforce Burnout Crisis: Exploring Signs and Solutions attendees on Nov. 9.
The session presented a range of strategies to support professionals, especially those in ED and ICU environments. The complete webinar can be reviewed here. It is presented at no cost as part of HASC’s Care for the Caregiver initiative.
The presentation slide deck is also available here and below.
Workforce burnout is hitting hospitals in a big way, said Jeannine Loucks, a Providence St. Joseph Medical Center mental health nurse supervisor who also teaches at U.C. Irvine and Golden West College. One study found 67 percent of frontline workers “screened positive for burnout.” Additionally, twice as many workers are now citing retirement as reason for leaving — versus career or other motivations, ED manager Shela Kaneshiro told the group.
Burnout also impacts hospitals through increased leave time taken by employees and increased overtime hours. But there may be an upside to current conditions.
The challenges presented by COVID may also be strengthening team bonds, Trudy Johnson of Dignity Health California Hospital Medical Center noted.
On a recent survey, “the positive was (employees) felt very strongly about their teamwork and their coworkers,” Johnson said. ”We also saw improvement in people knowing how to escalate patient safety issues.”
Evidence is also accumulating that strategies can mitigate stressors and build resilience for frontline teams.
“It’s really important to examine our own vulnerabilities, to know our own triggers,” Loucks explained.
The ability to compartmentalize helps those in high-stress fields when one case is finished — before moving to the next individual who needs care, she said.
Similarly, the practice of mindfulness, which connects one to the present to buffer them from rumination and worry, is a proven method for reducing stress.
Facilities can offer meditation led by a facilitator — or via an app or online videos, Kaneshiro said. Another approach is a designated pause following a negative outcome. Orange Coast Medical Center staffers often call a Code Lavender following a death or other event, Kaneshiro related.
Other support methods link impacted employees with team members like therapists, HR managers and chaplains. Coworkers and hospital administrators also lend support via longrunning Tea for the Soul and similar programs.
Additional strategies and practices are listed in the Nov. 9 webinar recording — and on HASC’s Care for the Caregiver page. Feel free to share the page link with others who may find it useful: www.hasc.org/post/care-caregiver-resources.
HASC plans to present additional webinars focused on workforce burnout solutions throughout the year. Contact education program manager Jamila Mayers to learn more.
Contact:
Jamila Mayers
(213) 538-0739
jmayers@hasc.org



